Download The Free Guide Here
Receive the guide by email and be kept updated on other clinical resources.
The Hard Part Is Not Recognizing Harm. It Is Knowing When It Meets the Threshold for Trauma Exposure.
Clinicians are often clear that something harmful has occurred. What is less clear is whether an experience rises to the level of trauma exposure as it is defined clinically. Trauma does not always arrive as a single, overt event. It is often relational, cumulative, and shaped by power, threat, and limited options for safety. Without a clear framework, clinicians are left to rely on intuition, event severity, or heuristic shortcuts to make that determination.
That uncertainty matters. When trauma exposure is underrecognized, treatment may miss its mark. When it is named prematurely, clients can feel mischaracterized or pushed before they are ready.
This checklist was created to support careful assessment by giving clinicians a structured way to think, so they can determine when trauma exposure is present without rushing, minimizing, or overpathologizing.
Why This Uncertainty Carries Clinical Risk
When clinicians do not have a solid way to assess trauma exposure, the effects are often subtle but far reaching. The question “Does this count” quietly shapes everything that follows, from diagnosis to treatment planning to how clients understand their own experience.
Without a clear assessment framework:
- Trauma exposure may go unrecognized and therefore untreated
- Trauma may be over identified, disrupting treatment fit and pacing
- Clients may internalize clinician uncertainty as minimization or invalidation
- Diagnosis and documentation may become inconsistent or defensively vague
A clear assessment framework does not force conclusions. It reduces guesswork. It allows clinicians to move forward with greater precision, confidence, and alignment between formulation and care.
What This Free Guide Helps You Do
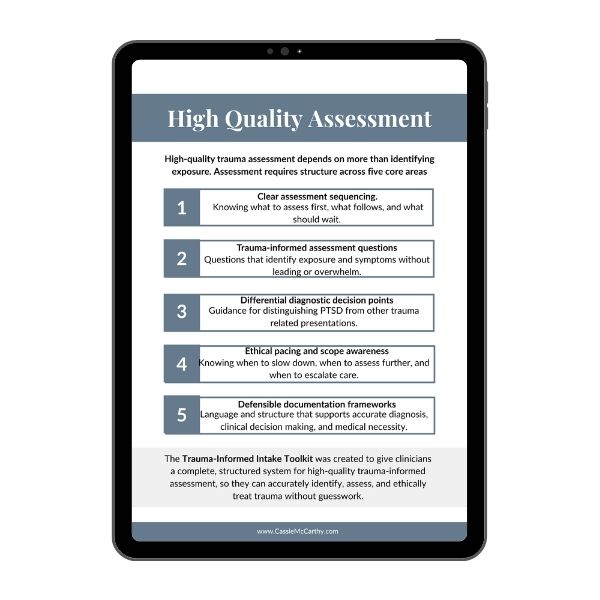
This checklist is designed to support clear, grounded clinical decision-making when trauma exposure is uncertain. It provides a structured way to assess whether an experience meets the threshold for trauma exposure, without relying on event severity alone.
By working through the prompts, clinicians can systematically evaluate contextual threat, power dynamics, and constraints on choice that are often missed in standard intake processes. The checklist helps clarify whether trauma exposure is present, unclear, or unlikely, and whether further assessment for PTSD or other commonly occurring trauma related conditions is warranted.
Rather than forcing labels or conclusions, the checklist supports careful assessment so clinicians can move forward with greater clarity, consistency, and confidence in formulation and next steps.
Access the Free Guide Here
You’ll receive the checklist by email, along with occasional clinician-focused resources. Unsubscribe anytime.
How to Use This Free Guide
This checklist is meant to support your clinical thinking when trauma exposure is uncertain. It offers a structured way to assess whether an experience meets the threshold for trauma exposure and whether further trauma related assessment may be needed. It is designed to fit into intake and ongoing formulation, not to replace comprehensive assessment or clinical judgment.
The checklist is not a diagnostic tool or trauma screener, and it does not tell you how to label a client’s experience or what treatment to provide. Its purpose is to reduce guesswork, not override your expertise, so you can move forward with greater clarity and confidence.
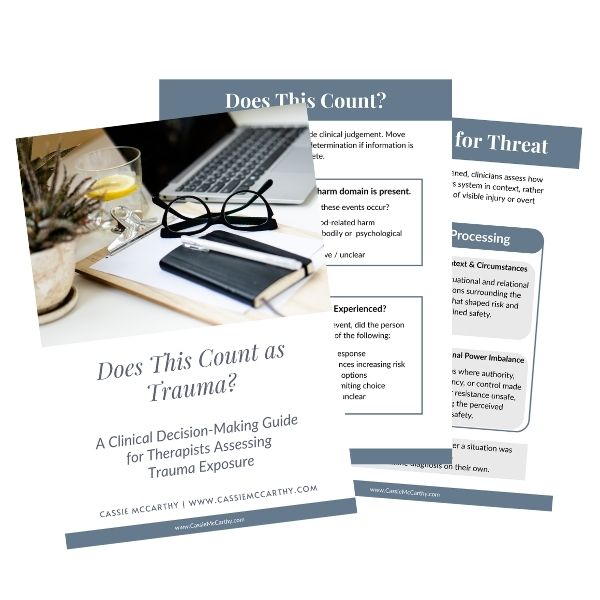
What’s Inside:
This guide walks clinicians through a structured, step by step process for assessing trauma exposure when the answer is not immediately clear. It is designed to be used sequentially, without forcing conclusions when information is incomplete.
Ready?
Inside, clinicians are guided to:
- ☑️ Identify whether a qualifying harm domain is present, including death or livelihood related harm, serious bodily or psychological injury, or sexual harm
- ☑️ Assess whether threat was experienced at the time, using contextual factors such as autonomic threat response, power differentials, and lack of safe or viable options
- ☑️ Distinguish between actual and threatened harm, recognizing that trauma exposure is defined by how survivability was appraised in context, not by hindsight or visible injury
- ☑️ Clarify next steps, including when trauma exposure is met, when further assessment is needed, and when symptoms may be better explained by other clinical factors
The guide emphasizes that trauma exposure is one component of formulation, not a diagnosis, and supports ethical pacing by helping clinicians decide when further assessment for PTSD or other trauma related conditions is warranted.
Who This Is For
This guide is designed for clinicians who regularly encounter uncertainty when assessing trauma exposure. It is especially useful when harm is interpersonal, relational, subtle, or ongoing, and when clients present with anxiety, depression, or distress that does not fully explain their history.
Ready?
This tool may be a good fit if you:
- Work with clients who wonder whether what they experienced was “bad enough” to count as trauma
- Find yourself unsure whether to name trauma exposure, assess further, or slow down
- Want a structured way to evaluate exposure without minimizing or overpathologizing
- Value ethical pacing, diagnostic accuracy, and clear clinical reasoning
This guide is intended for licensed mental health clinicians and trainees practicing within a clinical setting.

Created By
Cassie McCarthy, LICSW is a trauma therapist and clinical educator specializing in interpersonal trauma and PTSD. Her work focuses on improving how trauma exposure is defined, assessed, and treated in clinical practice, particularly when harm is relational, ongoing, or difficult to classify.
This checklist reflects her clinical experience working with trauma presentations that are often minimized or misdiagnosed, as well as her commitment to evidence based trauma treatment and ethical, precise assessment.
Stop relying on intuition. Start using a grounded framework to support your clinical reasoning today.
You’ll receive the checklist by email, along with occasional clinician-focused resources. Unsubscribe anytime.
Looking for the Client Version?
Want a tool to help your clients understand whether they may have experienced trauma, in their own language and at their own pace?
There is a separate client facing version of the “Does This Count as Trauma?” tool designed for psychoeducation and self understanding. This page is for the clinician version, which is built for professional assessment and clinical reasoning.
If you are looking for something to share directly with clients, the client tool is the appropriate option.